Causes of Hypoxemia
This is the eighth video in our Pulmonary and Ventilator Mechanics Chalk Talk Series, where our goals are to learn how a ventilator works, and how to work a ventilator. In this talk, we take a close look at the five causes of hypoxemia: hypoventilation, insufficient inspired oxygen, diffusion limitation, ventilation-perfusion mismatch, and shunt.
Hypoventilation & Low PiO2
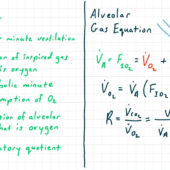
As we saw in the last lecture, the alveolar gas equation explains the decrease in alveolar -- and therefore arterial -- oxygen partial pressure in hypoventilation and insufficient inspired oxygen pressure. Hypoventilation itself has myriad causes, from decreased central drive to breathe in narcotic overdose to peripheral issues such as neuromuscular disorders, and various intermediate states like obesity hypoventilation syndrome and chronic obstructive pulmonary disease. Insufficient inspired oxygen partial pressure falls under high altitude -- mountaineering and aviation mishaps -- and low inspired oxygen fraction -- limited to certain scuba diving or respirator accidents.
In this lecture, we will answer two questions about each cause of hypoxemia: First, is there a difference between the alveolar and arterial oxygen partial pressure -- also called an A-a gradient? Second, does supplemental oxygen improve the hypoxemia? For both hypoventilation and low inspired oxygen, the alveolar gas equation tells us that there is no A-a gradient and that supplemental oxygen does correct the hypoxemia.
Diffusion Insufficiency
In the normal alveolar capillary, mixed venous blood from the pulmonary artery enters the capillary. As it transits the pulmonary capillary -- usually over the course of 1/4 to 3/4 of a second -- the gas in the alveolus diffuses into equilibrium with the capillary blood. After it exits the pulmonary capillary, the blood is arterial.
Thus, there are two primary mechanisms of diffusion insufficiency: First, if diffusion itself is limited -- usually due to the proliferation of the shared basal lamina between pneumocytes and capillary epithelium caused by pulmonary fibrosis -- the capillary blood may not reach equilibrium with alveolar gasses before it exits the capillary. Second, if the capillary transit time is extremely rapid -- which requires an increase in heart rate and cardiac output generally only obtainable at the Olympic athlete level -- the capillary blood may not have time to equilibrate with alveolar gas despite normal diffusion speed.
The more common clinical scenario is a combination of these pictures: a patient with moderate to severe pulmonary fibrosis may have diminished diffusion speed between the alveolus and capillary, but has clinically acceptable gas exchange at rest. When that patient gets up to walk, however, the increase in cardiac output results in just enough decrease in pulmonary capillary transit time that hypoxemia is the result. This is corrected by supplemental oxygen.
Insufficient diffusion by definition causes a difference between alveolar and arterial oxygen partial pressures, so there is an A-a gradient. And because supplemental oxygen drives the gradient -- and therefore diffusion speed -- higher, it does correct the hypoxemia of diffusion insufficiency.
V-Q Mismatch
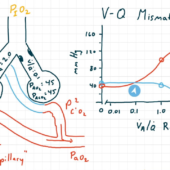
All of the causes of hypoxemia we have looked at so far -- hypoventilation, reduced inspired oxygen pressure, and diffusion limitation -- we have been able to explain using a very simple, single-compartment lung model. To explain ventilation-perfusion mismatch, or "V-Q mismatch," we need to make our model a little bit more complicated. In this model, the pulmonary artery splits into two pulmonary capillaries, each of which diffuses perfectly with its own distinct alveolus before recombining into oxygenated, arterial blood at the pulmonary vein.
Ventilation-perfusion mismatch arises when the share of ventilation by breathing gas in these two alveoli differs from the share of pulmonary perfusion of their respective capillaries. This physiology arises in practically any pulmonary disease, but is classically seen in obstructive diseases such as emphysema In our example, we look at two segments with equal blood flow but unequal ventilation.
What makes analysis of this situation tricky is that each alveolus will have a different oxygen and carbon dioxide partial pressure, dependent on its exposure to mixed venous blood and fresh breathing gas. Those calculations can't be written down as a simple equation, but some common sense and computer modeling can help us find the values.
As the capillary blood from each alveolus recombines into arterial blood, we need to consider the oxygen and carbon dioxide content in the blood -- rather than simply the partial pressure -- to determine the partial pressures in the resultant arterial blood.
One further trick in ventilation-perfusion mismatch is calculating the alveolar-arterial gradient. If every alveolus has a different oxygen partial pressure, what do we use to compare with arterial oxygen? The answer is that we use the ideal calculated alveolar partial pressure, which is the result of the alveolar gas equation calculated with the measured arterial carbon dioxide partial pressure substituted for the alveolar carbon dioxide partial pressure.
With this in mind, ventilation-perfusion mismatch does have an A-a gradient. Because supplemental oxygen increases the alveolar partial pressure in all ventilated alveoli, it improves end capillary oxygenation even in low-ventilation segments, and therefore does improve the hypoxemia.
Shunt
Shunt is a special case of ventilation-perfusion mismatch, in which a lung segment receives no ventilation at all. The hypoxic vasoconstriction reflex in the pulmonary vasculature works to decrease V-Q mismatch generally and shunt specifically, but when that reflex fails or is overwhelmed, shunt can be the result.
Intrapulmonary shunt is evident when some alveoli are filled with fluid, such as in bronchial pneumonia or ARDS. Shunt can also arise due to arterovenous malformation, congenital heart defect with Eisenmenger physiology, or other pathways. Everyone has some degree of shunt caused by the bronchial circulation and the Thebesian veins.
The behavior of shunt and its mathematical explanation are very similar to that of V-Q mismatch. The big difference is that capillary blood in the shunt segment is not exposed to alveolar gas at all. For that reason, supplemental oxygen does not improve the hypoxemia of shunt.
We've now reviewed the relationship between ventilation and hypercarbia, as well as the five causes of hypoxia: hypoventilation, insufficient inspired oxygen, diffusion limitation, ventilation-perfusion mismatch, and shunt. Going forward, we will look at how we optimize ventilator therapy to correct hypoventilation and hypoxemia.

Comments
This post currently has no responses.