Patient-Triggered Breaths
This is the fifth video in our Pulmonary and Ventilator Mechanics Chalk Talk Series, where our goals are to learn how a ventilator works, and how to work a ventilator. In this talk, we add one more bit of complexity to our ventilator modes: patient interaction. Patient-triggered breaths are critical in encouraging patients to breathe synchronously with the ventilator. They reduce the work of pulmonary musculature, and provide a pathway to weaning off a ventilator.
Assist & Assist/Control
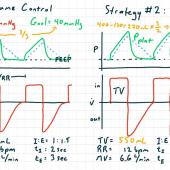
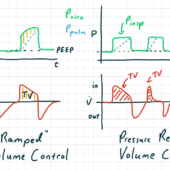
Assist modes, such as pressure assist and volume assist, are identical to their respective control modes with one important difference: instead of breaths being triggered by a timer which is programmed to a respiratory rate, breaths are triggered by patient effort. The ventilator recognizes patient effort either by the decrease in circuit pressure -- a pressure trigger -- or forced inspiratory flow -- a flow trigger -- that results when a patient "sucks" on the endotracheal tube when exerting inspiratory effort.
Assist/control are both time-triggered and flow- or pressure-triggered. This means that patients are free to initiate breaths, but if the patient's breath initiation is slower than the programmed respiratory rate, the ventilator will trigger "control" breaths.
It's important to realize that in assist, control, and assist/control modes, the breaths themselves, in terms of inspiratory limit and cycle to expiration, are exactly the same. The patient begins a breath, but the length and nature of inspiration remain programmed.
Pressure Support
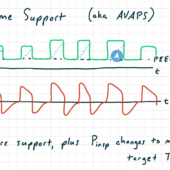
Unlike assist modes, pressure support allows the patient both to trigger a breath and to cycle to expiration. As its name suggests, pressure support is a pressure-limited mode with a set inspiratory pressure. The patient triggers breaths with a flow or pressure trigger just like in assist modes. After initial, high inspiratory flow starts, the cycle to expiration occurs when inspiratory flow drops below a given threshold.
In pressure support mode, the patient has a lot of volitional control over their ventilation. By increasing or decreasing their own compliance using their respiratory musculature, they can increase or decrease their tidal volume dramatically. This makes pressure support a very comfortable ventilator mode.
IMV and SIMV
Next, we think about the development of intermittent mandatory ventilation (IMV). In the earliest control modes of ventilation, the inspiratory valve could not open during the expiratory phase. That meant that if the patient tried to inhale during the expiratory phase, they would be inhaling against a closed valve, spending respiratory effort with no flow. That was both psychologically distressing in the case of light sedation, and contributed to respiratory muscle weakness. Under IMV, the patient was "allowed" to take breaths, without any support, during the expiratory phase.
This progressed to synchronized intermittent mandatory ventilation (SIMV), under which the ventilator would detect inspiratory effort that was near in time to its next planned, time-triggered inspiration. When detected, the ventilator would trigger its breath slightly early, assisting with ventilator synchrony.
SIMV w Pressure Support
The most common modern version of SIMV is pressure-supported SIMV. In these modes, the ventilator delivers two distinct kinds of breaths: control breaths are still delivered on schedule as programmed. If the patient exerts inspiratory effort between control breaths, their efforts are supported by pressure support, with a programmed inspiratory pressure, just like if they were on pressure support mode. This is a very frequently used mode in today's intensive care units.

Comments
This post currently has no responses.