Setting the Vent II: Oxygenation
This is the tenth video in our Pulmonary and Ventilator Mechanics Chalk Talk Series, where our goals are to learn how a ventilator works, and how to work a ventilator. This time, we look at the nuts and bolts of treating oxygenation both by increasing mean airway pressure using PEEP, as well as by working with inspired oxygen fraction. We look at the risks of ventilator induced lung injury.
Preliminary Questions
Before looking more directly at correcting hypoxemia, we address three preliminary questions that help to clarify our approach.
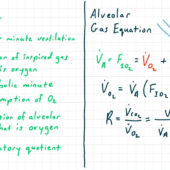
First, if FiO2 and airway pressure are both in the alveolar gas equation, why does increasing FiO2 help so much in insufficient PiO2, hypoventilation, and diffusion limitation, but increasing airway pressure does not?
The answer is that on the scale of barometric pressure -- 760mmHg at sea level, the pressure that can be added with a ventilator -- even 15mmHg (20cmH2O) is relatively high -- is insignificant. Compare that with FiO2, which can be easily tripled or quadrupled with a ventilator, and you see the discrepancy.
Second, if that's the case, why does increasing mean airway pressure always seem to help oxygenation in real life?
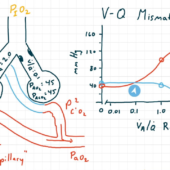
The answer here is that increasing mean airway pressure improves ventilation-perfusion matching, and V/Q mismatch is always present in hypoxemia, especially when there is any pulmonary disease present. Increasing mean airway pressure also recruits atelectatic lung segments, further improving V/Q matching.
Finally, in the list of mechanisms of hypoxemia, why do we specify "true" shunt?
The answer is that in pulmonary physiology, "shunt" can mean two different things. In "true" shunt, as we saw in lecture 8, mixed venous blood proceeds to the left heart without coming into contact with alveolar gas, either because of complete obstruction of airflow (e.g. in purulent pneumonia) or because it bypasses the alveolar capillary entirely (e.g. in an arteriovenous malformation). However, we often simplify ventilation-perfusion mismatch into a three-compartment lung model, in which case "shunt fraction" is a measure of both "true" shunt and low V/Q segments. Their response to intervention, as we know, is different.
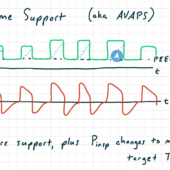
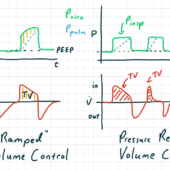
↑ PEEP
To increase mean airway pressure, we almost always go with the strategy of increasing positive end-expiratory pressure. This has the net effect of increasing all absolute pressures (PEEP, peak, plateau, and mean airway pressure) by a uniform amount. If the patient stays in a linear compliance domain, the driving pressure, tidal volume, and minute ventilation will not change significantly. The biggest trade-off here is that by increasing plateau pressure, we have increased risk of lung injury.
Vent-Induced Lung Injury
To understand these trade-offs, it's time to introduce the basics of ventilator-induced lung injury. This topic will be covered in more detail in a future lecture. Barotrauma is the overdistension of lung with breathing gas, which is more likely with higher plateau pressures. At the extreme, it can cause pneumothorax, pneumomediastinum, and air gas embolism. Volutrauma is lung injury caused by the stretch of large-volume inhalation and exhalation over time, and is made worse by large tidal volume and driving pressure. Atelectotrauma is caused by alveoli opening and closing with every breath; risk is increased at low PEEP, which allows more lung segments to collapse. These pressure-related lung injuries, in addition to hyperoxic lung injury and ventilator-associated pneumonia, are the biggest risks to patients arising from mechanical ventilation.
PEEP Rules of Thumb
There are some targeted techniques, like stress index, that help optimize PEEP in challenging situations. For most patients, however, you can get by with a few rules of thumb.
- Start with a PEEP (in cmH2O) equal to the patient's BMI (in kg/m2) divided by 4, and plan to increase from there. A significant part of the reason for PEEP is to counteract the weight of the chest wall and abdominal tissue during expiration, so bigger patients need more PEEP.
- If you increase PEEP and measured compliance increases, you are probably on the right track. Modern ventilators display a measured compliance with every breath. Increasing compliance with increasing PEEP shows that you are moving to a more favorable domain of pulmonary mechanics.
- If you increase PEEP and measured compliance decreases, you might be approaching the patient's plateau pressure limit. As you can probably intuit, at the high end of the patient's pulmonary pressure and volume capacity, elastance increases and compliance decreases. If you increase PEEP and notice that compliance decreases, you might be getting there.
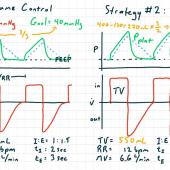
↑ P-insp
You could also increase mean airway pressure by increasing inspiratory pressure. We usually don't do this for several reasons. First, the increase it provides to mean airway pressure is tiny compared to increasing PEEP. Second, it much more dramatically increases ventilation, so if your PaCO2 was already dialed in precisely, it will throw that off. Third, its risk profile is unfavorable: compared to a situation of increased PEEP, increased inspiratory pressure carries the same risk for barotrauma, and higher risk of volutrauma and atelectotrauma.
↑ I:E Ratio
One more option to increase mean airway pressure is to increase the inspiratory-to-expiratory time ratio. Although this provides only a very modest increase to mean airway pressure, it does so essentially "for free." As long as the I:E ratio is kept low enough to keep auto-PEEP at bay, adjusting it upward will not increase risk of lung injury or other complications.
Inspired Oxygen Fraction
Our other big tool to increase arterial oxygen is the inspired oxygen fraction, FiO2. In most cases, high FiO2 is enough to correct hypoxemia, but that must be balanced against the risk of hyperoxic lung injury.
Hyperoxic lung injury clinically presents like ARDS, and is both dose- and time-dependent. Even at 100% FiO2, most patients won't experience issues until 24 hours of exposure, and most patients won't suffer from hyperoxic lung injury at FiO2 less than 60%.
The evidence on exceptions to the general principle of "use the minimum FiO2 possible" is slim, but you will find people advocate for higher PaO2 -- even if it means higher FiO2 -- in patients with ongoing ischemia or hymodynamic instability with threatened watersheds. We should be especially careful to keep FiO2 low after reperfusion, in neonates, and in patients who have ever been exposed to bleomycin, a chemotherapeutic drug.
At this point, we've finished the first "chapter" of the Ventilator and Pulmonary Mechanics Chalk Talk Series, and you should be well equipped with the foundations for employing mechanical ventilation for a patient with reasonable pulmonary physiology. Going forward, we will be examining patients with more extreme physiology, including the acute respiratory distress syndrome, severe obstructive disease, and morbid obesity. In order to tackle those problems, we'll be taking deeper dives into physiology topics -- like chest wall compliance -- and technology topics -- like non-conventional ventilation modes and different breathing gasses -- that complete the mechanical ventilator toolkit.
Comments
This post currently has no responses.