Compliance and Resistance
This is the second video in our Pulmonary and Ventilator Mechanics Chalk Talk Series, where our goals are to learn how a ventilator works, and how to work a ventilator. In this talk, we explore the concepts of compliance and resistance and some of the pathology associated with each. We investigate peak pressure and plateau pressure as tools to differentiate between low-compliance and high-resistance pathology, and finally consider auto-PEEP, or "breath stacking," as a complication of mechanical ventilation.
Resistance
We begin by diving into the definition of resistance covered in the first lecture: the proportionality constant that determines how much pressure is needed to generate a given level of flow from one point to the other. In a simplified system of a cylindrical tube with laminar flow, Poiseuille's Law tells us that the resistance to gas flow through the tube is proportional to the length of the tube, and inversely proportional to its radius to the fourth power. We use this approximation conceptually in airway mechanics, with the conclusion that airway edema or bronchoconstriction, especially in pediatric cases, can lead to significant increases in resistance.
Turbulent flow comes into play at high airway velocities and high resistance. Though we are going to put turbulent flow aside for the foreseeable future, it is likely present in most ventilation, and does play a significant role in high-resistance disease states like asthma.
Compliance
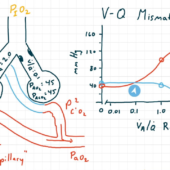
Up until this point, we've taken it on intuition that the pressure in the lungs increases as you add air. The relationship between pulmonary pressure and volume is called compliance, and represents the stress/strain relationship or "stretchiness" of the lungs. A lung with low compliance requires a lot of pressure to inflate, which leads to unfavorable physiology.
Compliance isn't exactly linear, especially at the low (atelectatic) and high (overpressure) ranges of the pulmonary pressure-volume curve, but we hope to mostly work in that linear region.
Resistance and Compliance
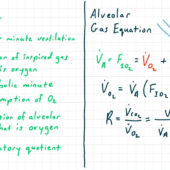
By adding the equations for compliance and resistance, we get one of the fundamental equations that describes the behavior of circuit (or airway) pressure in the ventilator-patient system. Namely, circuit pressure is going to two ends: first, to overcome resistance and contribute to flow through the airways; and second, to overcome elastance (the inverse of compliance) and distend the lungs.
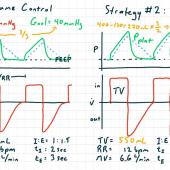
Peak & Plateau Pressure
One clinical diagnosis problem that comes up in ICUs and operating rooms is: the ventilator's circuit pressures have increased, and we wonder whether the clinical problem is one of increased resistance -- which might indicate asthma, COPD, airway swelling, or a kinked endotracheal tube -- or one of decreased compliance -- which might be a sign of pulmonary fibrosis, edema, increased abdominal pressure, or bronchial intubation.
We tease out the difference in behavior of these clinical entities by performing an inspiratory breath hold to determine our peak pressure and plateau pressure. Increased resistance will cause high peak pressure with normal plateau pressure, while decreased compliance will increase both peak pressure and plateau pressure.
Auto-PEEP
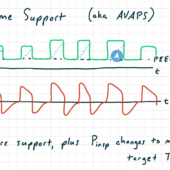
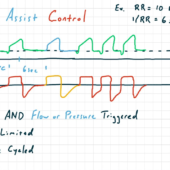
Finally, we look at our first complication of mechanical ventilation, auto-PEEP or "breath stacking." Auto-PEEP occurs when the expiratory time on the ventilator is insufficient -- either because it was set too short by the operator, or because expiration is slowed by high resistance, or some combination of the two. This results, especially in volume control modes, in a consistently increasing pulmonary and circuit pressure as the lungs do not empty with every breath.
Auto-PEEP is best avoided by ensuring adequate expiratory time, by using modest respiratory rates and low inspiratory to expiratory time ratios when possible. When it occurs, auto-PEEP can progress to hemodynamic compromise, as pulmonary pressure is transmitted to the thorax, resulting in decreased venous filling. In an emergency, this can be relieved by disconnecting the expiratory limb of the ventilator from the endotracheal tube, allowing for full expiration and hemodynamic recovery.

Comments
This post currently has no responses.